The annual HIMSS conference always sparks lively discussions among the HIT community about innovative technology and the role it will play in patient care. While this year’s event held similar discussions, what stood out is that providers, payers and vendors seemed unusually anxious, concerned, and excited about two areas expected to drive the next great wave of digital health innovation – Artificial Intelligence (AI) and smart Siri-like assistants called “chatbots” – and it’s easy to understand why.
The Anxiety: The community recognises that healthcare innovation lags behind other industries, and there’s dire need to move faster. No one echoed this point better than Rebecca Kaul, chief innovation officer at MD Anderson. During her keynote at a Sunday Summit she the audience that, “We’ve all seen what happens when companies get too complacent in their success. Remember Blockbuster Video? Remember when everybody had a Blackberry?” The health IT community wants to innovate faster. They see that Amazon, Google and Facebook have already started to disrupt consumer expectations once again, now with AI-rich, conversational experiences. Providers and payers know this drill. Consumer experiences will quickly translate into new expectations from their patients, members and employees. Herein lies their source of anxiety – because innovation efforts compete for resources with mandatory ‘run-the-business’ projects that address a new government’s policies, increasing security and privacy threats, and issues like interoperability.
The Controversy and Concern: The AI discussion became embroiled in controversy from the get-go. In 2016, Artificial Intelligence (AI) and chatbots rapidly rose to the media forefront after Facebook, Amazon, Google, Microsoft, IBM and other tech giants announced investments and released products to market. The HIMSS conference keynote, led by IBM CEO Virginia Rometti, reflected the healthcare industry’s growing excitement about the role AI can play with clinical diagnosis, treatment and beyond. Yet in a bout of unfortunate (and seemingly coincidental) timing, the most prominent AI project in healthcare, a nearly $40M union between IBM and MD Andersen, came toppling down as Forbes first released news that MD Anderson Benches IBM Watson In Setback For Artificial Intelligence In Medicine. It’s not surprising to see healthy scepticism, especially when you couple this news with ethical questions about how AI will affect human jobs and negative press surrounding Facebook Messenger bots or the Microsoft Tay debacle.
The Excitement: Despite the rational questions surrounding these technologies, it was clear that people expect ground-breaking impacts to be made for patients, caregivers and complete industries workforce. Sessions on AI and chatbots literally had an overflow of people in the hallways. Numerous large payers, pharmaceutical companies and providers shared that they now have “teams dedicated to their AI and chatbot projects.” For this enthusiastic and innovative audience, there was no question whether AI and chatbots will be used. They simply wanted to know where they should start. From medical diagnosis and disease prevention to use cases that improve productivity, care coordination and employee experiences, to opportunities to better engage patients or members, the industry knows there are endless possibilities ahead with this technology.
Also Read: How Chatbots are Positively Impacting Healthcare Sector |
How to Approach the Innovation Challenge and Opportunity
HIT leaders need to determine whether to lead or follow in this paradigm shift. To reduce the anxiety and controversy and prepare for success, here are three pieces of advice.
1. Understand how to articulate the value of AI-rich, conversational interfaces
Let’s cover a few undebatable facts:
- Clinicians are stretched for time. Studies show that for every one hour physicians provide direct clinical face time to patients, nearly two additional hours are spent on EHR and desk work per day.
- Provider and payer staff waste time on inefficient processes, manual tasks and slow forms of communication. The diverse system environments created by complex business partnerships and ongoing M&A hinder workforce productivity, especially for tasks that require provider-to-provider and provider-to-payer interaction.
- Patient and family engagement is constrained by today’s digital environments. Healthcare ‘self-service’ experiences still leave much to be desired. Less than 30 percent of potential users have adopted patient portals, which is a problem considering healthcare providers represent the top industry for expensive call centers.
Kicking off the UX Forum at HIMSS, a UX expert reminded the audience of a simple reason for the aforementioned facts: “Healthcare is late to the game in terms of user experience. Patients are tired of impersonal and hard to use portals. Surveys show problems with UX for clinical documentation and nursing: too many clicks required by EHRs, poor templates that affect data quality, difficulty in communicating context and design-hampered challenges with workflow and care-coordination”.
Something must change. Here’s why intelligent, conversational UIs help:
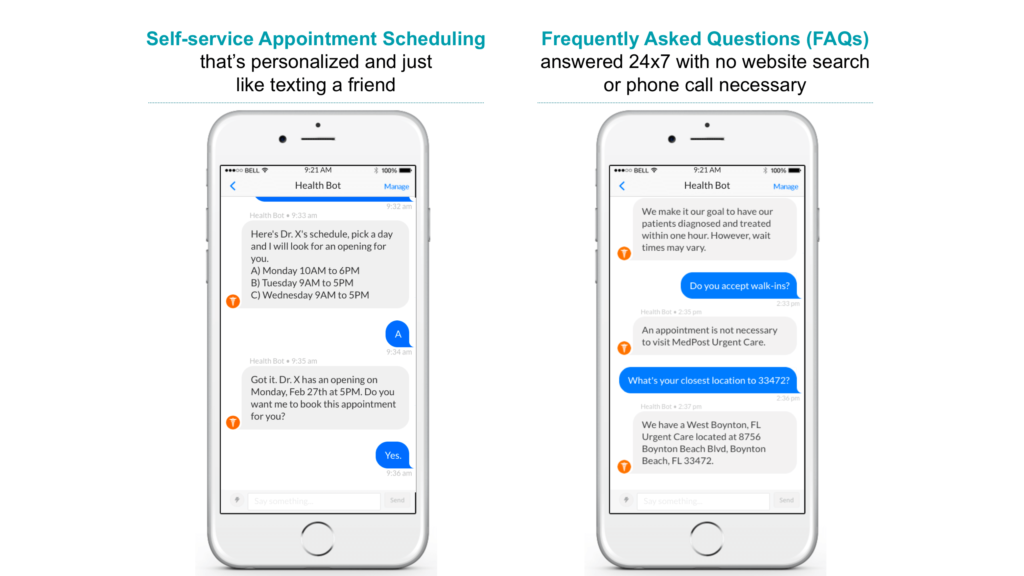
- The UI is “no UI” Unlike applications or portals that each have different graphic user interfaces (GUIs), a conversational chatbot facilitates a person-to-system interaction in channels people already use to communicate with friends or colleagues – SMS, e-mail, Facebook Messenger, Spark, Skype etc. Chatbots can also live in existing websites, portals or mobile apps. The interface also remains the same as people complete tasks across different systems, like entering data into an EMR or requesting time-off. This means there’s little training needed, and no toggling from one app to the next.
- They facilitate a natural language based conversation via speech or text. Traditional GUIs require users to understand each individual application feature – where to click, what fields to enter, what actions to take and what to do next. A conversational chatbot eliminates clicks, screen searching and form fields, allowing people and systems to simply speak or text in natural language to get something done. That’s why tasks can be completed in a fraction of the time.
- AI can be applied with chatbots to quickly to make systems more helpful to humans. Today’s static systems receive data and use it to process a singular action. While they hold patient, employee and company-specific information, that information is static and rarely remembered in context. They also can’t “feel” or “learn” from successes and failures. Chatbots can be designed with AI capabilities so they remember and use contextual data – such as a patient’s facility preferences or a nurse’s preferred shifts – both in the short term or long term. They can also use sentiment analysis to understand and respond to human emotions and learn from conversations to get better over time.
Also Read: Say No to Infodemic: How Healthcare Virtual Assistant Acts as a Perfect Response Assistant |
2. Be realistic about AI projects for clinical diagnosis
We all wish for AI to find cures to diseases, change health outcomes and save people’s lives. It’s human nature. While it’s not far-fetched to expect that AI will uncover patterns that aid in medical diagnoses, the HIT community must recognise that there are implications due to the high-risk nature of this AI use case.
Compliance and ethics teams will be vocal stakeholders in projects. Clinical teams will actively engage to analyse results before a single conclusion ever gets made, let alone applied. New technology skills, teams or large consulting engagements will be required. The technology will be tested in hundreds of ways, with mass amounts of training data required for every instance – a challenge given the variances in how medical information gets recorded and stored.
If you dig under the covers of the MD Andersen and IBM project, this seems to be the root of the problem. It’s like introducing a child to jigsaw puzzles and starting with the most difficult 500-piecer you can find.
Challenges don’t mean healthcare you shouldn’t pursue AI for clinical diagnosis. But you must prepare for what could be a controversial and costly journey that takes years to drive measurable impact.
3. Consider ways to drive immediate impact from AI chatbots
Much like I shared in a December article for IT Pro magazine, the HIT community should remember that innovation doesn’t have to make headlines or be the subject of lengthy news features. It just has to work. The realistic and immediate AI and chatbot use cases may not cure diseases, but they can help drive smarter and faster decisions, and remove time-consuming, administrative burdens that hinder patient engagement and quality of care. Here are just 2 simple examples:
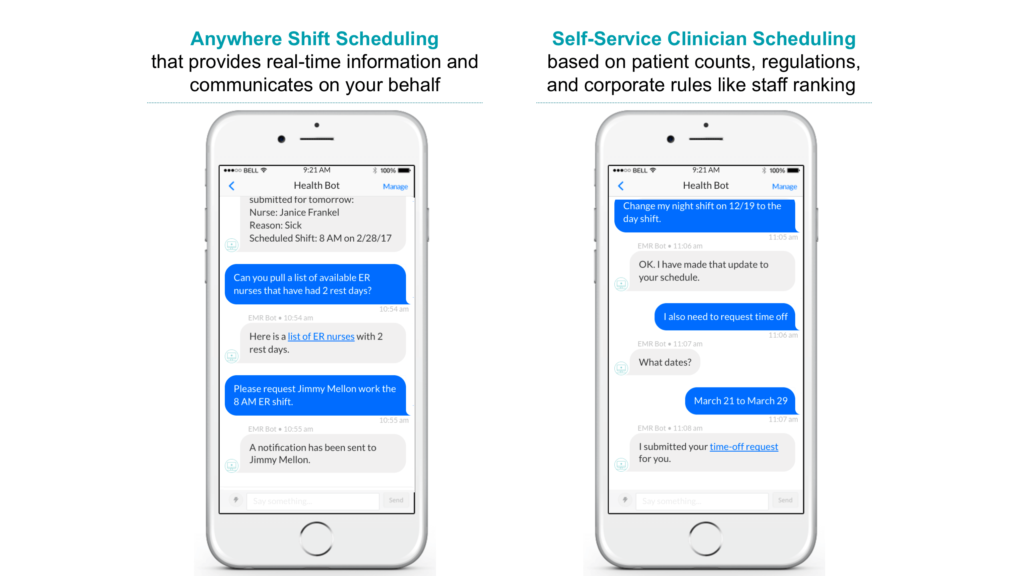
Patient engagement. It’s proven that when patients engage, it creates a measurable impact on healthcare costs and outcomes. Recent studies show that unengaged patients are three times as likely to have unmet medical needs, and two times more likely to defer care. Providers also save millions of dollars when patients use portals for areas like scheduling of doctor’s visits, FAQs, online billing inquiries and lab results. That’s why these are some of the most common initial tasks providers are pursuing with intelligent chatbots.
Clinical scheduling. Clinical managers can spend more than 50 percent of their time each day working to address daily staffing imbalances and subsequent regulatory, cost and retention concerns. This is why software providers like Infor and Kronos enriched their software with robust analytics tools that help managers understand these situations. But managers and clinical staff need still need ways to respond faster, on-the-go, and in a self-service fashion. That’s why scheduling is one of the top use cases for AI and intelligent chatbots.
Also Read: How Retailers Can Win Millennials’ Business – And Everyone Else’s While They’re at It |
The Great Lesson of History
Major innovations like AI and conversational interfaces bring about skeptics and believers. Will systems really be smarter than humans? Will people really want to “talk” more than they text? I’d suggest that we ask a different question based on history’s greatest lessons: Will this technology create a way of doing something that’s simpler, faster or smarter than how we do it today? To that question, the simple answer is yes. History proves that human nature will always lead us to that end. We stopped using horses and buggies when we could use cars. We replaced manual farming with tractors that produced a higher yield.
Today, intelligent conversational experiences represent our future. They will streamline, humanise and improve how people interact with systems and machines. Here’s to betting healthcare leaders break through the hype, understand what’s possible and become leaders not laggards at this momentous time.